
Dr Michael Yeadon: Veliko prepozno, če ga še niste videli, ampak kadarkoli slišim Vallance Waffle- a govoriti o virusih & mutantih, grem in poiščem pravega strokovnjaka. PV ne ve nič več o tem kot jaz. Razlika je v tem, da jaz ponujam strokovnjake, da se pogovorijo z vami. Vallance je sramota za glavnega znanstvenika.
Vir: https://twitter.com/MichaelYeadon3/status/1346936739336695817
Dr Michael Yeadon: Obstajajo velike težave s strašenjem z "mutantom" koronavirusa SARS CoV-2. Ni dokazov, da je bolj nalezljiv. Ferguson je bil avtor tehnične note, ki je bila obravnavana s strani NERVTAG (New and Emerging Respiratory Virus Threats Advisory Group) , nato na SAGE (vladna znanstvena svetovalna skupina za nujne zadeve), ki je obravnavala oceno prejšnjega, nato na TV.
Vir: https://twitter.com/MichaelYeadon3/status/1347853988352454656
*

By Vincent Racaniello - http://www.virology.ws/about/, CC BY 3.0, https://commons.wikimedia.org/w/index.php?curid=34878931
*
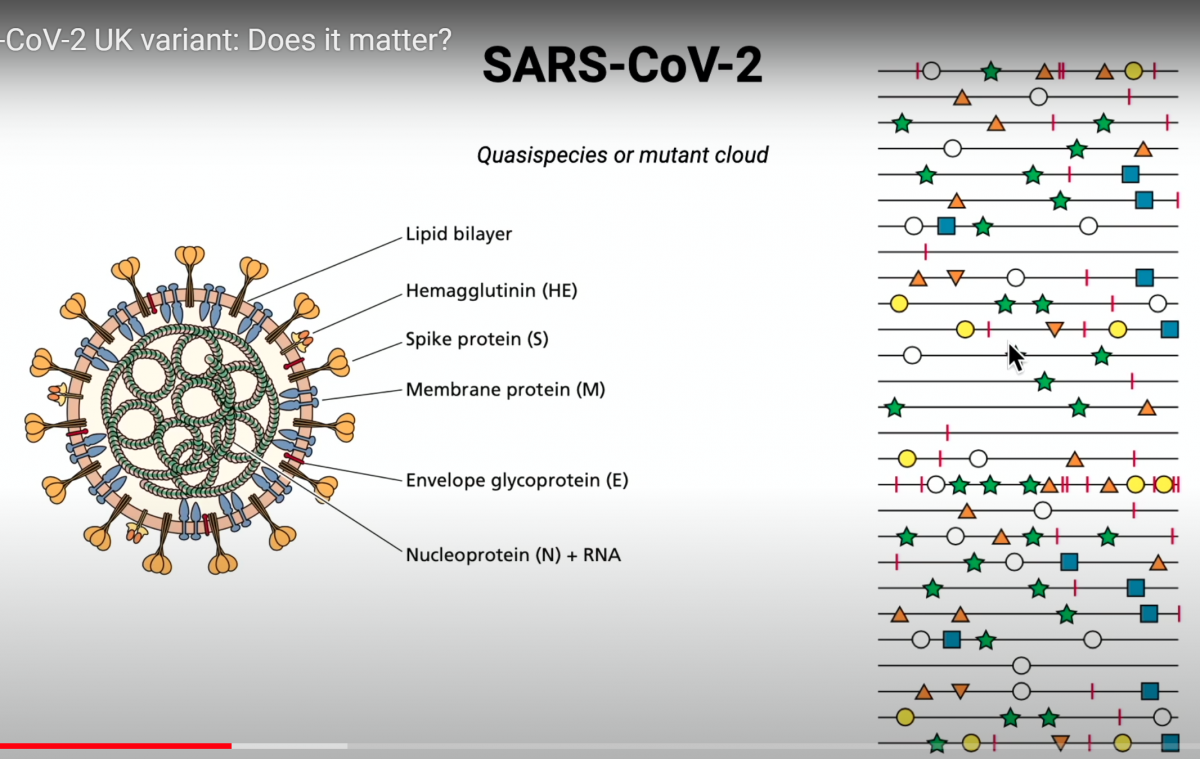
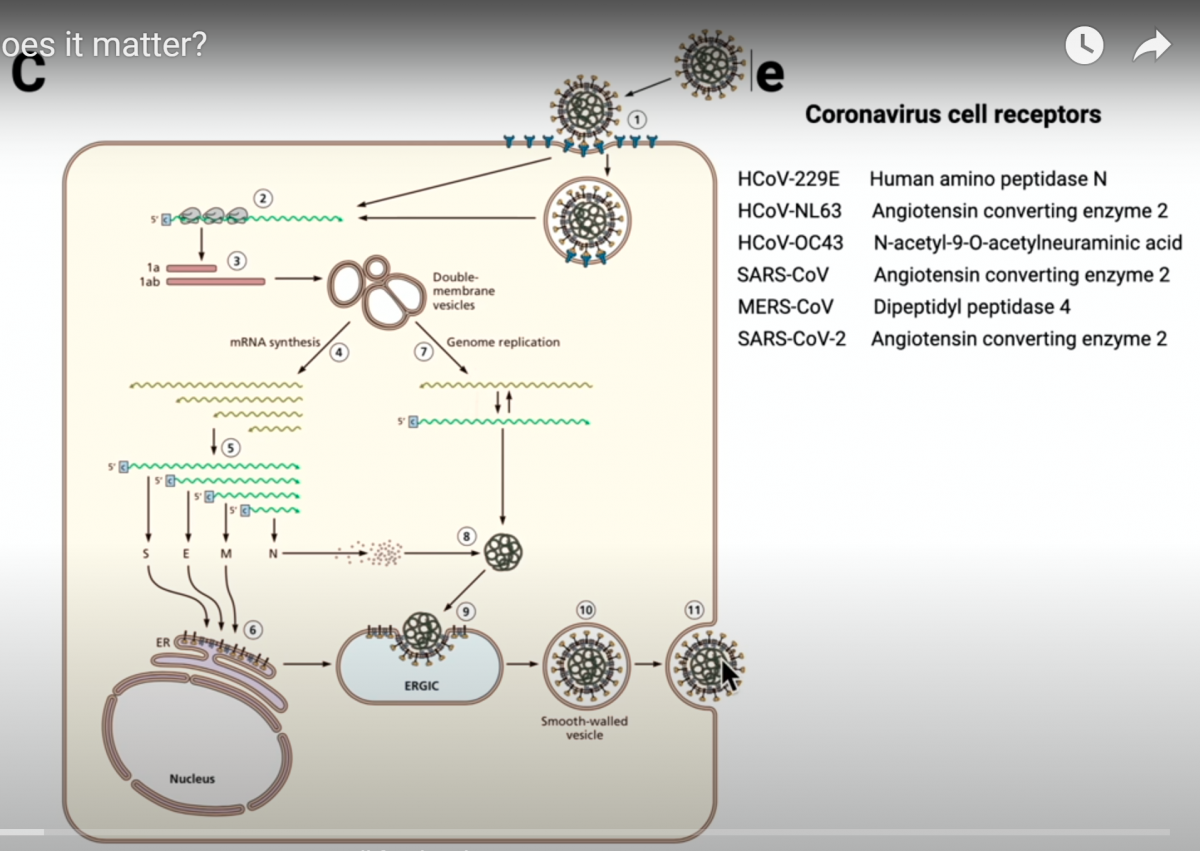
Prof. dr. Vincent Racaniello: Virusi mutirajo več čas. Vsak genom vseh živih bitij ima mutacije ob vsakem ciklusu replikacije, ker encimi polimeraze naredijo napake pri prepisovanju/ kopiranju. RNA virusi so znani po tem, da zelo pogosto mutirajo, ker imajo slabši mehanizem popravila napak v genomu ali ga sploh nimajo. Bakterije pa imajo nizko stopnjo mutacij.
RNA koronavirusi imajo velik genom - okoli 30.000 baznih parov nukleinskih kislin in imajo mehanizem za popravilo napak, zato imajo srednjo stopnjo mutacij genov. A še vedno imajo približno 1 mutacijo na 10.000 ali 20.000 baz pri replikaciji RNA genoma. To pomeni, da se v celici ob replikaciji koronavirusa dogaja veliko mutacij in vsak bazni par virusne RNA se lahko zamenja/ mutira.
*
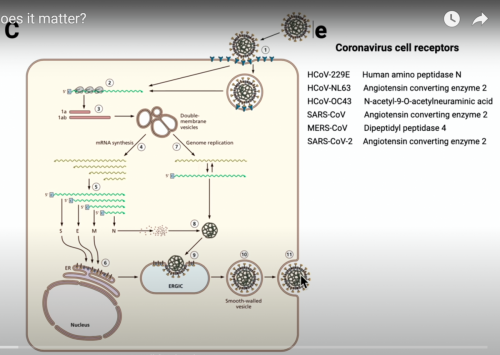
replikacija koronavirusov
*
Vsakič ko se virusna RNA replicira znotraj celice, nastane določeno število napak/mutacij. V eni sami celici nastane več tisoč virusov, ki so kolekcija mutantov. Koronavirus SARS CoV-2 ima velik genom- okoli 30.000 genov in vsakič ko koronavirusi pridejo ven iz celice, je med njimi zelo veliko mutantov. To kaže naslednja slika- linije na desni predstavljajo genom koronavirusa SARS CoV-2 in simboli na liniji kažejo različne mutacije.
*
Mutacije koronavirusa SARS CoV-2
*
Nekatere mutacije so za virus smrtonosne, ker onemogočijo reprodukcijo virusa, ko vstopi v naslednjo celico. Mnoge mutacije so nevtralne, nekatere pa imajo učinek. Do sedaj so mutacije koronavirusa SARS CoV-2 imele minimalni učinek na lastnosti virusa in niso vplivale na potek COVID-19 bolezni. Če bi se zgodila takšna mutacija, bi nov mutirani virus imenovali "nov sev" (angl.: strain). A do zdaj nimamo nobenih novih sevov koronavirusa SARS CoV-2, ampak samo variacije ali variante genoma prvotnega virusa.
Torej virusi vedno mutirajo, vprašanje pa je, ali mutacije povzročijo spremembo v aminokislinah virusnih beljakovin. Do sedaj so znanstveniki našli 12.000 mutacij v 90.000 izoliranih koronavirusih SARS CoV-2. Vsak izoliran virus se od drugih razlikuje v približno 10 nukleotidih. Nobena od teh mutacij pa ni vodila v nov sev koronavirusa SARS CoV-2, ki bi imel drugačne biološke lastnosti. Nobena mutacija izmed 12.000 ni povzročila sprememb v prenosljivosti okužbe med ljudmi niti v patogenezi. Torej te mutacije niso povzročile nobene bistvene posledice. To velja tudi za zadnjo mutirano inačico koronavirusa SARS CoV-2, ki je bila izolirana v Veliki Britaniji. Zelo težko je uporabiti epidemiološke podatke, ki predstavljajo širjenje virusa v populaciji in zaključiti, da se nova inačica koronavirusa širi bolj kot prejšnje. Virusi, ki pridejo ven iz bolne osebe so mešanica različnih mutiranih koronavirusov. Vendar bolna oseba prenese na drugega le del te mešanice, ki ima določen set mutacij. Vsak okuženi bo tako imel mešanico mutantov in tako imenovan "učinek ustanovitelja" (founder effect). Spremembe se dogajajo naključno in nimajo bistvenega učinka, a se lahko zdi, da se širijo ponekod hitreje, a v resnici ni tako.
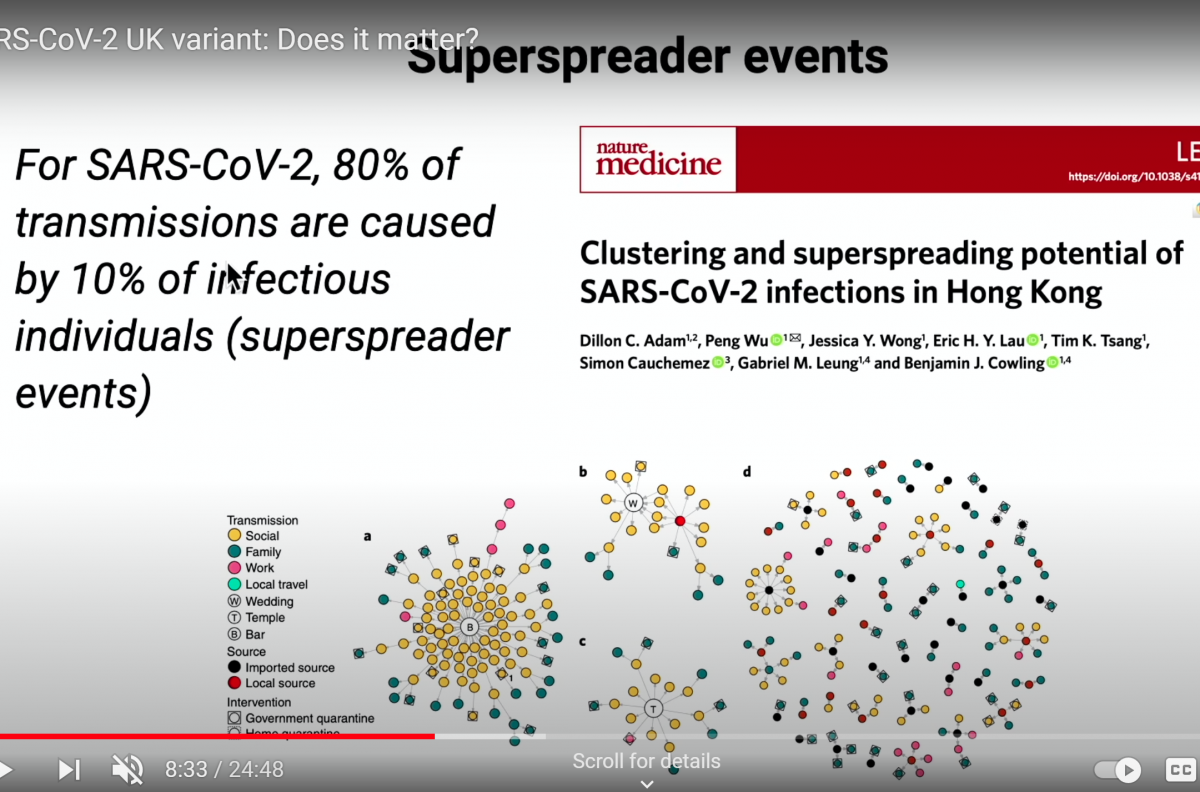
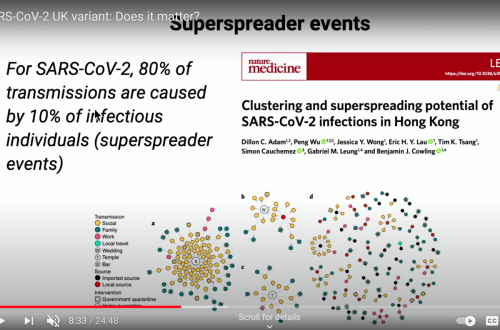
COVID-19 se širi preko precej majhnega deleža populacije, a hitrejše širjenje ni posledica novega- mutiranega genoma koronavirusa, saj je znano, da večino okužb širijo t.i. "super prenašalci" na določenih skupnih dogodkih.
*
80% transmisij SARS CoV-2 koronavirusa povzroči 10% okuženih posameznikov, ki so t.i. "super prenašalci" na določenih skupinskih dogodkih, kot so poroke, cerkveni obredi, bari ali restavracije. Slika kaže v sredini leve skupine enega okuženega (B)- founder effect, ki okuži veliko drugih ljudi, ki potem okužbo širijo dalje. Če je ta en okuženi imel mutacijo genoma, ki povzroča na primer spremembo v aminokislini v belajkovinski bodici (spike gliko proteinu), potem bo imelo mnogo okuženih ljudi ta mutiran virus, kar prestraši medije, kot se je zgodilo zdaj v Veliki Britaniji. A v resnici je večina mutacij brez posledic.
Slovenski mediji so poročali:
V Angliji so zaznali nov sev koronavirusa. Okuženih je že preko 1000 ljudi, virus pa se predvsem na jugu Anglije širi eksponentno. Vlada je zato že zaostrila omejevalne ukrepe. Zaprli so tudi bare in restavracije. Kakšno bolezen povzroča novi virus ni znano, zaenkrat pa ocenjujejo da naj ne bi povzročal hujše oblike bolezni covid 19.
Vir: https://www.domovina.je/v-angliji-nov-sev-koronavirusa-zaostrujejo-ukrepe/
Kaj se je torej zgodilo v Veliki Britaniji?
*
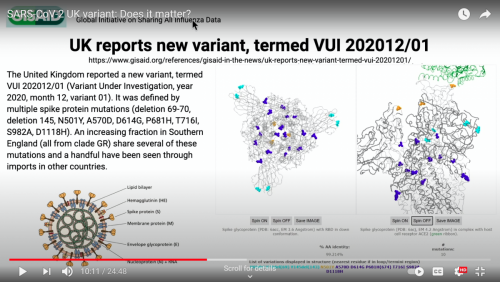
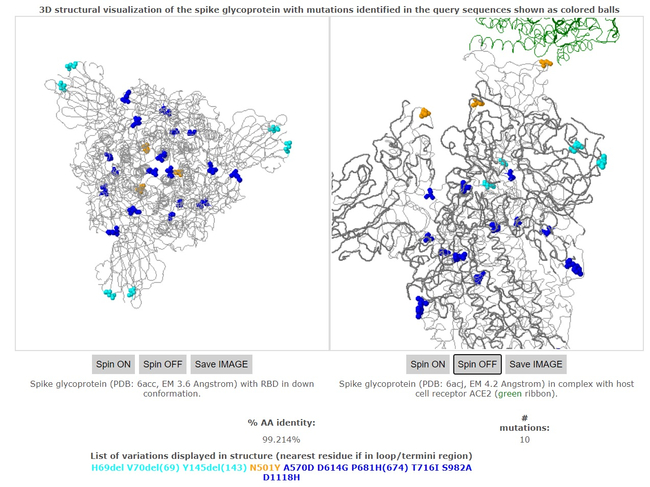
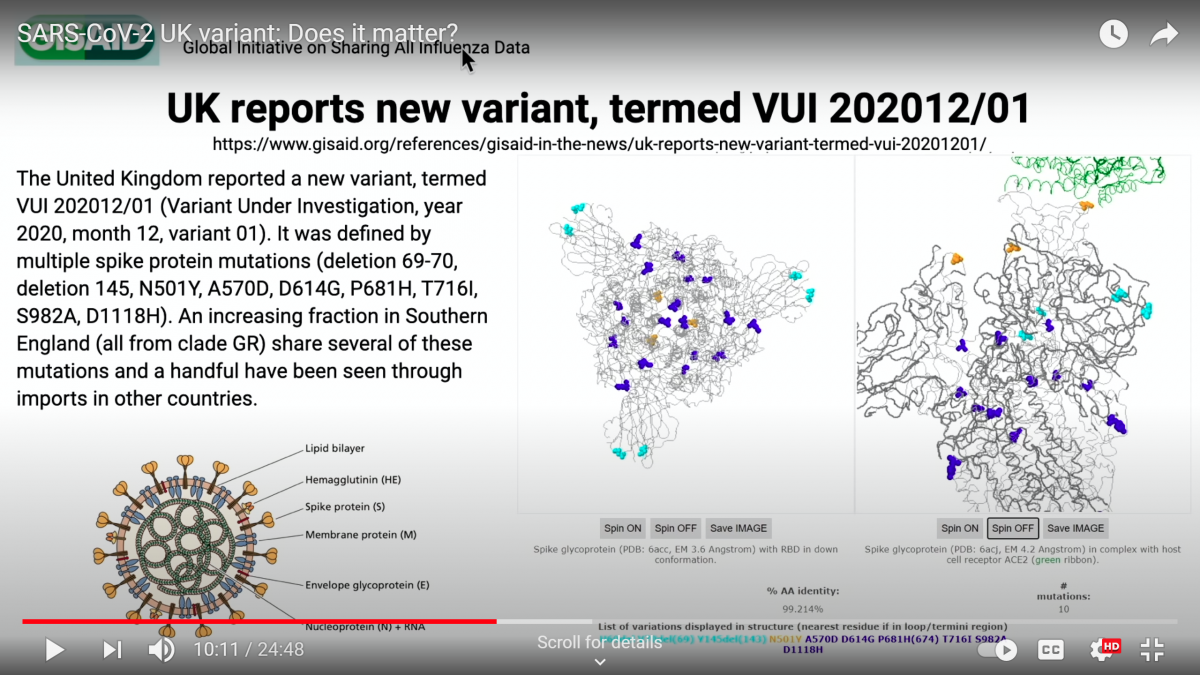
Iz Velike Britanije poročajo o mutirani inačici z imenom VUI 202012/01, ki ima spremembe v več aminokislinah beljakovinske bodice: tri aminokisline so izbrisane, šest jih je spremenjenih
*
Vse dosedanje inačice koronavirusa se nahajajo v podatkovni bazi na naslovu:
https://www.gisaid.org/references/gisaid-in-the-news/uk-reports-new-variant-termed-vui-20201201/
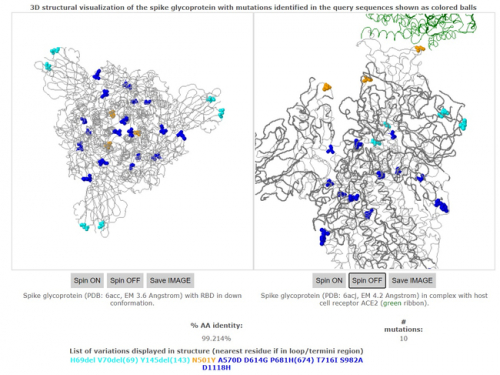
VUI 202012/01 mutacija beljakovinske bodice koronavirusa SARS CoV-2
*
Beljakovinska bodica je zelo pomembna, saj omogoča virusu, da okuži človeške celice. Ima tri polipeptidne verige, ki jih prikazuje zgornja slika. Zelena barva označuje mesta, preko katerih se koronavirus SARS CoV-2 veže na receptorje v membrani človeške celice. Označene so tudi spremembe aminokislin. Ena izbrisana aminokislina je na mestu vezave virusa, zato se lahko sprememni moč vezanja. najbolj pomembna sprememba je verjetno v aminokislini N501Y (oranžne barve), na mestu vezave na človeško celico in vezave protitelesa. Druge mutacije aminokislin so manj pomembne. Izbris ORF8 beljakovine se je zgodil že prej tudi v Singapurju, kar je precej oslabilo patogenost (virulenco) virusa, vendar mediji o tem nikoli ne poročajo. Nikakor ne moremo zaključiti, da se nova inačica koronavirusa SARS CoV-2 hitreje širi kot prejšnje.
18. decembra 2020 je bilo srečanje NERVTAG (New and Emerging Respiratory Virus Threats Advisory Group- svetovalna skupina za nove in nastajajoče grožnje respiratornih virusov), kjer so obravnavali novo mutacijo koronavirusa SARS CoV-2. V skupini je tudi Neil Ferguson iz Imperial College London, ki je dal popolnoma napačen model pandemije v začetku leta 2020. Sprejeli so dokument, ki je prestrašil svet. Največja koncentracija novega mutanta je v Londonu, razširila pa se je tudi v druge države. Dokument navaja, da je korelacijska analiza pokazala povečanje v R vrednosti (0, 39-0,93). R pomeni indeks reprodukcije ali koliko drugih ljudi bo okužila ena okužena oseba. Za SARS CoV-2 naj bi veljalo, da ena okužena oseba povprečno okuži dve ali tri druge osebe, če ni lockdowna, mask, razdalje ali drugih ukrepov. NERVTAG skupina je torej zaključila, da število R narašča pri tej novi inačici virusa. Vendar je napačno uporabiti epidemiološke podatke, da bi sklepali o bioloških lastnostih virusa. Zato so potrebni eksperimenti. Zato je NERVTAG napačno sklepal, da gre za povečanje transmisije virusa. To je neznanstveno in napačno. (lažna ali pseudo znanost).
Drug sklep skupine se nanaša na RT PCR testiranje. Cycle treshhold = Ct vrednost praga ciklov pove, koliko kopij RNA je v vzorcu. NERVTAG je navedel, da se je Ct vrednost zmanjšala za dva cikla pri novi inačici virusa. Ct razpon je od 11 do 35. Pri 11 ciklih RT PCR testa, če je pozitiven, imamo v vzorcu veliko virusne RNA, če pa je RT PCR test pozitiven pri 35 ciklih, pa ima vzorec iz testirane osebe zelo malo virusne RNA, in oseba po vsej verjetnosti ne bo kužna (ne bo virusa prenašala na druge ljudi). NERVTAG skupina je sporočila, da se je Ct znižal za dva cikla, kar naj bi pomenilo, da je v testiranem vzorcu več virusne RNA, kar naj bi spet pomenilo, da se virus v celicah bolj reproducira. Iz nosa osebe vzamejo vzorec virusne RNA, jo spremenijo v DNA in pomnožijo in potem izračunajo število kopij RNA, ki so bile prvotno navzoče v nosu testirane osebe. To se imenuje virusna obremenitev (viral load). NERVTAG je sporočil, da se je virusno breme povečalo za 0,5 v povprečnem logu10, glede na virusno breme Y501 v primerjavi z N501.
Zaključek skupine NERVTAG je bil: NERVTAG zmerno zaupa, da VUI-202012/01 kaže znatno povečanje prenosljivosti v primerjavi z drugimi variantami virusa"
V tem sta dve napaki: "zmerno zaupanje" in "znatno povečanje". Za to ni dokazov, na voljo so imeli posredne podatke, ki ne dokazujejo ničesar. Ct vrednost se lahko spremeni tudi zaradi drugih vzrokov, ki vplivajo na transmisijo in ne moremo sklepati, da je vzrok sprememba v virusu. RT PCR test pa je sam po sebi napačen. Z njim ne morete meriti infektivnosti virusa. Če bi želeli ugotoviti, ali se nova inačica virusa res hitreje prenaša, bi morali izmeriti infektivnost virusa. RT PCR testa tega ne meri. Nekdo ima lahko na primer inačico koronavirusa SARS CoV-2, ki naredi več majhnih delčkov RNA v inficiranih celicah. In potem bi imeli nižjo Ct vrenost RT PCR testa. Zato je zaključek skupine NERVTAG popolnoma nepravilen in to je popačena znanost, ki na osnovi Ct vrednosti sklepa, da je nov mutant bolj prenosljiv.
NERVTAG je tako zaključil, da trenutno ni dovolj podatkov, da bi lahko ocenili mehanizem domnevno povečanega prenosa virusa in ali je potek COVID-19 bolezni hujši (bile so 4 smrti na 1000). Vendar je resnica, da za zdaj še ni znano. ali se nova inačica koronavirusa SARS CoV-2 res hitreje prenaša. Sprememba je v enem epitopu izmed 20 epitov, ki so na površini koronavirusa- epitop je del virusa, ki ga prepoznajo celice našega imunskega sistema (predvsem B ali T celice) in zato ni verjetno, da bi sprememba enega epitopa spremenila odziv imunskega sistema na nov mutiran virus.
Virus se bolj prenaša, če je na primer v nekem okolju bolj stabilen ali če bolnik oddaja več virusov v okolje. Vse to se lahko izmeri. Vendar NERVTAG nima namena izvajati teh testov, sekvencioniranje in RT PCR test pa niso dokaz, da je nova inačica virusa bolj prenosiljiva kot druge. Problem je tudi v tem, da ko jemljejo bris iz nosu, dobijo od vsake osebe drugačno količino testnega vzorca. Pred časom je krožila po svetu inačica koronavirusa SARS CoV-2 D614G in tudi takrat so na podoben način strašili ljudi in govorili, da se bolj prenaša. Niso pa naredili pravilnih poskusov, da bi to tudi dokazali in tako je tudi v sedanjem primeru.
Jaz sem profesor virologije Vincent Racaniello in hvala, da ste me poslušali.
Vincent R. Racaniello, higgins profesor na oddelku za mikrobiologijo in imunologijo univerze Columbia, univerze za zdravnike in kirurge, ZDA Je soavtor učbenika o virologiji- Principles of virology
Vir: https://www.youtube.com/watch?v=wC8ObD2W4Rk&feature=emb_logo
*
Nervtag had identified a new variant of the novel coronavirus in the South East of the country, which was 70% more transmissible than its predecessor, carried a viral load up to 10,000x higher and which the primer on the widely used Thermo Fisher TaqPath PCR machines failed to pick up.
https://lockdownsceptics.org/the-glitch-that-stole-christmas/
*
*
*
https://www.regionalobala.si/novica/krek-svari-ce-se-bo-razsirila-angleska-razlicica-virusa-bomo-ze-konec-meseca-v-tezkem-epidemioloskem?fbclid=IwAR1ccJfVEvYN-WqWT5azb1H6xF8MyiOW7TTrD7AJu5nLDfpOwed9vwdUxSI
*
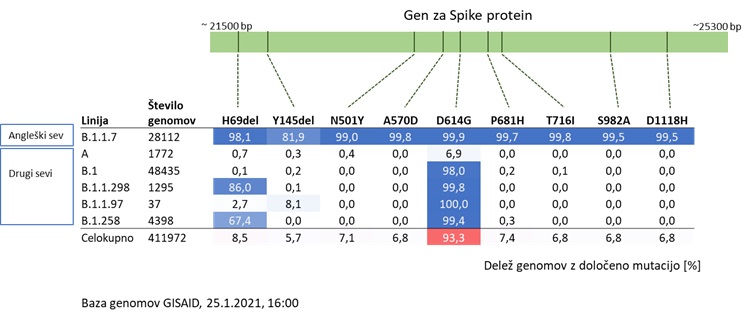
Čeprav je za angleško različico (imenovano tudi B 1.1.7) značilnih 23 sprememb, je vseeno tako, da posamezna sprememba ni prisotna v 100 % pri vseh virusih angleške različice.
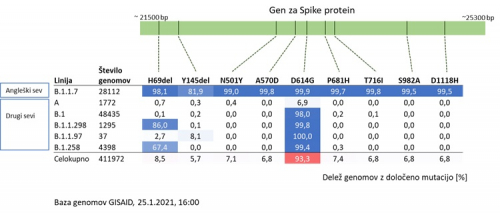
Da je virus v vzorcu angleška različica, lahko z največjo gotovostjo trdimo, če določimo celotni dedni zapis virusa v vzorcu in če se ta genom uvrsti v linijo B.1.1.7.
Ker pa je postopek branja dednega zapisa virusa v vzorcu bolnika (ali sekvenciranje) dolgotrajen postopek, lahko uporabljamo tudi druge načine. Vendar so ti drugi načini manj natančni in zato samo presejalni. To pomeni, da iz vseh pozitivnih vzorcev izločijo tiste, ki so verjetno angleška različica. Še zmeraj jih moramo potrditi z branjem celotnega dednega zapisa (sekvenciranjem), vendar na ta način močno zmanjšamo število vzorcev, ki jih je potrebno sekvencirati.
Eni od takih presejalnih testov so posebni PCR testi. Na tržišču jih zaenkrat ni veliko, saj je angleška različica sorazmerno nova, resnično problematična je postala v decembru 2020. Test slovaškega proizvajalca, ki se trenutno testira na NLZOH, deluje tako, da zaznava obe prvi spremembi v zapisu za bodico (H69del in Y145del). Kot je razvidno iz slike 3, je kombinacija teh dveh sprememb zelo pogosta pri angleški različici (B 1.1.7) in izjemno redka pri drugih različicah virusa. Rezultat tega PCR testa tako ni potrditev angleškega seva. Pač pa pozitivni rezultat samo pove, da je virus v vzorcu zelo verjetno angleški sev, kar pa je potrebno potrditi s sekvenciranjem.
* * *
How Worried Should We Be About the Variants?
by Dr Michael Yeadon and Marc Girardot
As the SARS-CoV-2 epidemic continues across the globe, many genetic modifications have started to appear in the virus. These are being sequenced, analysed1 and monitored by many scientists. This well known phenomenon occurs continuously for Influenza as well as for coronaviruses. Health authorities and mainstream media have been very wary of supposed heightened risk profiles of these new variants. They are also adamant about a potential risk of evasion from immunity, whether that immunity was acquired via infection or vaccination.
Some evolutionary virologists consider that viruses ‘attenuate’, or evolve towards less virulent forms. Some feel that novel pharmaceutical2 and non-pharmaceutical interventions3 – or specific circumstances4 – could possibly disrupt this evolutionary process and favour a more severe variant or threaten acquired immunity.
The recent downward trends5 in cases and in hospitalisations across the globe seem to indicate that the virus has probably not mutated in any way that would make it much more dangerous and that a healthy immune system is very capable of dealing with these new forms of the SARS-CoV-2 virus. Indeed, patients have been shown to recover naturally in most instances just like they did from the original form of COVID-19.6 The paucity of confirmed re-infections with the virus, accompanied by clinical symptoms, despite hundreds of millions of infections over the last year,7 is consistent with a lack of ‘immune escape’.
Acquired immunity is fundamentally based on the recognition of a large series of three-dimensionally shaped protein markers called ‘epitopes’. These markers are formed from a virus’s genetic code. When a virus mutates it can stop expressing some of these proteins, and, in principle, trump the immune arsenal specifically targeting these. And indeed, if all immunity against SARS-CoV-2 were based on one or two epitopes, and if those markers were to change, immunity would mechanically be broken.
But SARS-CoV-2 is a large virus8 with approximately 30,000 RNA bases (10,000 amino acids). Currently, the greatest difference between any ‘mutant variant’ and the original Wuhan sequence is limited to 26 nucleotide mutations.9 The genomic diversity of SARS-CoV-2 in circulation on different continents is fairly uniform.10 We know that the mutation rate in SARS-CoV-2 is slower than other RNA viruses because it benefits from a proofreading enzyme which limits potentially lethal copying errors.11 To date, these mutations have caused changes in less than 0.3% of the entire virus sequence. All variants are therefore currently 99.7% similar to the original Wuhan viral sequence.
To date, no robust scientific evidence proves that any of the variants identified are more transmissible or deadly than the original.12 By definition, variants are clinically identical. Once there is a clinical difference then a new ‘strain’ of virus has emerged. Prior knowledge of viral mutation shows they usually evolve to become less deadly and more transmissible.13 This optimises their chance of spreading, as dead hosts tend not to spread viruses, and very ill hosts have reduced mobility and thus limit contact with others.14
Natural immunity to SARS-CoV-2 is gained in the immune system by the body ‘cutting up’ the virus into hundreds of pieces.15 Multiple pieces are used to develop a suitably diverse immune response to many parts of the virus. Specialised immune cells16 will launch an immune response if exposed to the same ‘learned’ viral fragment in the future. Prior immunity gained from the original SARS-CoV-2 should work perfectly well against any new ‘mutant variant’, given the 99.7% sequence similarity.17
The La Jolla Institute for Immunology recently published a paper which is a tour de force: a comprehensive assessment of the role played by thousands of linear protein epitopes in the SARS-CoV-2 protein sequences18 in acquired immunity. Reassuringly, the human immune system uses several hundred of the theoretically possible protein epitopes. Each individual uses a diverse selection of at least 18 epitopes to form their antibody repertoire (humoral immunity)19, 20 and a different, though overlapping, T cell repertoire targeting at minimum 30-40 epitopes (cellular immunity).21 This means that even if there are several changes in the virus’s RNA code and in its protein sequence, the majority of the epitopes will be unchanged. There is therefore no possibility that the human immune system will be fooled into regarding the variants as a new pathogen. Furthermore, even if a variant were to bypass some of the immune repertoire of an individual, this would be of no consequence for a population, due to the diversity of repertoires. The authors themselves conclude: “This analysis should allay concerns over the potential for SARS-CoV-2 to escape T cell recognition by mutation of a few key viral epitopes.”
mRNA vaccines currently used for vaccination – Pfizer-BioNTech or Moderna – present the immune system with a large repertoire of targets, if not quite as large as a natural immune response. This is even more true of more traditional vaccines22 – Russia’s Sputnik and China’s Sinovac – which present an even wider repertoire.23 Given the breadth of immunisation and the relative independence of these immune responses, we believe that both humoral and cellular immunities will remain effective, even if one or several key immunological targets are erased.
Multiple confirming data points and experiments solidify this already robust scientific foundation: The prevalence of pre-existing immunity to SARS-CoV-2 found in multiple studies24,25,26 further validates our thinking, both for humoral immunity27,28 and cellular immunity.29 Many seem to have benefited from a form of immunity even though they had never met the actual virus, nor been vaccinated. These have gained their immunity from past epidemics and make up the large contingent of asymptomatics. The Tübingen University Hospital near Stuttgart, Germany found as much as 81% of its samples were carrying pre-existing specific T cells.30 Most likely, past common cold coronaviruses have – in effect – played an immunisation role against SARS-CoV-2. The same immunological mechanism has been proven to exist for influenza also.31
Some are advocating the vaccination of people who have recovered from COVID-19. Natural immunisation being the ultimate form of vaccination, we see absolutely no scientific nor medical justification for such a procedure. Even past infections by other forms of common cold coronaviruses have been found to protect from SARS-CoV-2. Injecting a vaccine should never be considered a trivial event. The decision should be based on a well thought out risk-benefit analysis. There is absolutely no patient benefit in vaccinating an immune person, only risks and possible unnecessary downsides32 such as fever.
The evidence above supports that immunity evasion – though a theoretical possibility – is very unlikely. Mutant variants, emerging overseas or domestically, are an inevitable biological reality once a virus is in the population. Closing international borders will not stop new mutations of the SARS-CoV-2 virus circulating in the population. It is a futile endeavour with no scientific basis.
Furthermore, immunity evasion may not be the most pressing issue with regards to COVID-19 and vaccine effectiveness. Could vaccines be partly ineffective for other reasons? Indeed, vaccines are different from drugs in that their mode of action is indirect.33 Vaccines rely entirely on a functional immune system. However, those suffering from severe forms of COVID-19 have predominantly been shown to be either very old and/or very sick with a weakened immune system.34 A recent survey from Yale University highlighted that blood samples taken from severe COVID-19 patients were lacking dendritic cells – a fundamental trigger of immune response – by a factor of between two and four.35 A deficiency in these signalling cells would thus significantly delay the immune response, giving the virus the opportunity to replicate exponentially, and present the immune system with a radically different context: a propagated virus and inflammation disseminated throughout the body. A vaccine’s mode of action would be subject to the same delay. Although vaccines could be helpful for patients with mildly deficient immune systems, they would most likely not save very old patients with advanced immune senescence. Thus overconfidence in vaccine effectiveness for the very old could be a major risk, and mitigation treatments and immune boosting strategies should instead be contemplated.36
Dr. Michael Yeadon
Scientific Board member of Panda
Expert in Allergy & Respiratory (A&R) Therapeutic/PhD in Biochemistry and Toxicology
Former Chief Scientific Officer at Pfizer A&R unit/CEO and Founder of Ziarco
25 years experience in Drug Discovery/40 Full Papers/63 Abstracts/two Books/six Patents
Marc Girardot
Member of Panda
Senior Advisor in Biotech & Automotive/INSEAD MBA
Advisor to an anti-Cancer therapeutic vaccine company/Ex-Global Lead of Cisco’s IBSG Automotive
30 years of experience in Industry, High Tech and Biotech/two Patents
https://lockdownsceptics.org/how-robust-is-covid-immunity/
*
https://www.bbc.com/news/world-asia-india-56517495
Mutacija v Indiji
*
Mutacija v Južni Afriki: https://www.rtvslo.si/zdravje/novi-koronavirus/v-juzni-afriki-potrdili-novo-razlicico-novega-koronavirusa/602663
*
*
Jan 09, 2021
